Polypharmacy and the Complex Maze of Drug Interactions in Pharmacovigilance
- 28/10/2024
In an era when patients, especially the elderly, are often prescribed multiple medications, polypharmacy has become a significant issue in healthcare. While these prescriptions aim to manage various coexisting conditions, they also present complex challenges. Polypharmacy is not just about multiple medications but the potential cocktail of interactions that can lead to adverse drug reactions (ADRs). Pharmacovigilance is pivotal in monitoring these risks, safeguarding patient health, and guiding healthcare providers through the intricate web of drug interactions.
What is Polypharmacy?
Polypharmacy typically refers to the concurrent use of five or more medications by a single patient. While it is often necessary to treat multiple conditions such as hypertension, diabetes, and arthritis, this practice increases the risk of ADRs, drug interactions, and medication non-adherence. Older people are particularly susceptible, as they are more likely to have chronic conditions requiring numerous drugs.
The issue doesn’t just lie in the number of medications but in the risk of interactions – drug-drug, drug-food, and drug-disease. These interactions can lead to diminished therapeutic effects or unexpected, harmful reactions, risking patient safety.
For instance, Figure 1 from the article by S. AlHarkan et al. illustrates the number of medications prescribed to patients. It shows that a significant number of them take more than 15 medications daily.
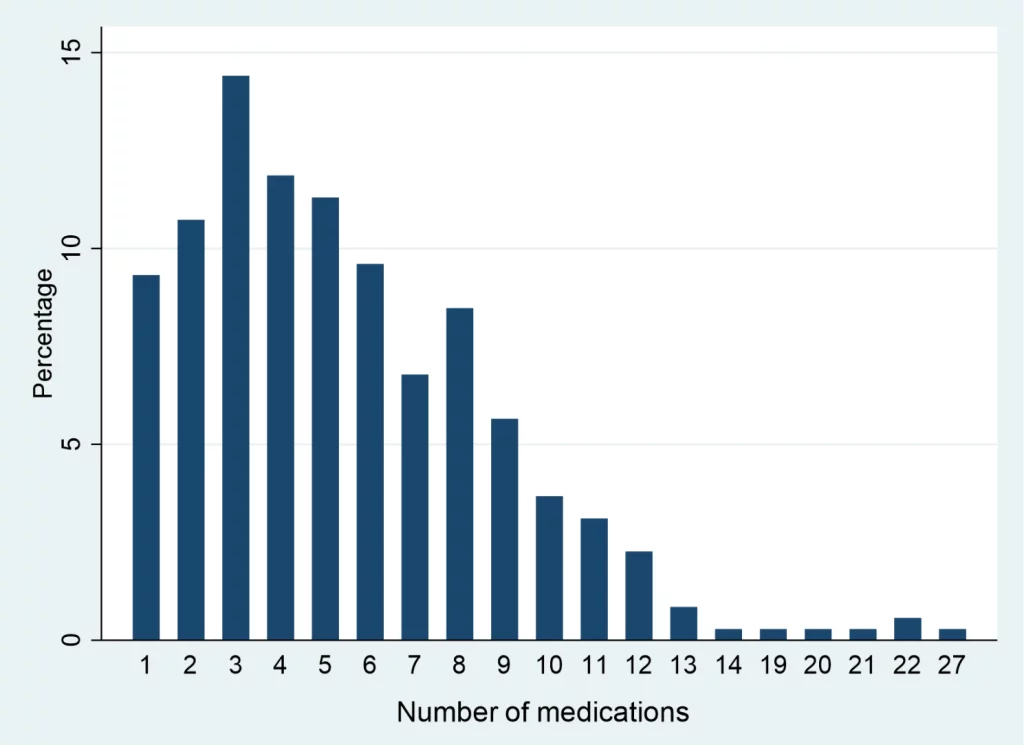
(Fig. 1. Adapted from the article by S. AlHarkan et al.)
The Role of Pharmacovigilance in Polypharmacy
Pharmacovigilance is the science of detecting, assessing, and preventing ADRs. With polypharmacy, the complexity of monitoring patient safety grows exponentially as each additional drug introduces new variables. A single new drug could trigger unforeseen interactions with the existing regimen, leading to adverse events that may not have been evident during clinical trials. Here’s where pharmacovigilance becomes critical.
Detection of ADRs
Real-world data from post-marketing surveillance helps pharmacovigilance systems detect ADRs that arise from polypharmacy. Since patients in clinical trials are often selected based on narrow criteria, the real-world scenario of patients on multiple drugs highlights risks not previously identified.
Signal Management
Pharmacovigilance systems continuously monitor for ‘signals’ – indications that a specific drug may be linked to an ADR. In cases of polypharmacy, signals related to drug interactions or additive side effects can emerge. These signals must be quickly investigated to understand their clinical significance and act accordingly.
Risk Minimization
When potential dangers related to polypharmacy are identified, pharmacovigilance initiatives focus on risk minimization strategies. This includes educating healthcare providers about possible interactions, adjusting dosing recommendations, or re-evaluating the need for specific medications.
The Hidden Dangers of Drug Interactions
Polypharmacy can obscure the root cause of an adverse reaction. For example, a patient may develop dizziness, but the true culprit could be the interaction between their antihypertensive and antidepressant. In such cases, isolating the ADR to a single drug is challenging, making pharmacovigilance efforts even more vital.
Moreover, many patients engage in self-medication with over-the-counter drugs, supplements, or herbal remedies, further complicating the picture. These substances, while perceived as harmless, can interact with prescription medications, increasing the risk of ADRs and complicating treatment.
Case Study: The Elderly Patient on Multiple Medications
Consider a typical elderly patient with hypertension, diabetes, osteoarthritis, and depression. This patient may be on a beta-blocker, a statin, insulin, a painkiller, and an antidepressant. While each drug is necessary, the combination increases the risk of interactions that may lead to ADRs, such as hypotension, hypoglycemia, or gastrointestinal bleeding.
Pharmacovigilance efforts here focus on continuously monitoring the patient’s response to the medication combination, adjusting dosages as needed, and educating both the patient and healthcare providers on the signs of potential ADRs.
Emerging Technologies: The Future of Pharmacovigilance in Polypharmacy
The rise of digital health technologies offers new tools for managing polypharmacy. Artificial intelligence (AI) can analyze vast datasets from electronic health records and pharmacovigilance databases to predict drug interactions. For example, tools like the DrugCard platform are already monitoring medical literature to detect unexpected ADRs and interactions, detecting potential dangers earlier than traditional methods.
As pharmacovigilance embraces these new technologies, we may see more personalized approaches to managing polypharmacy. By understanding a patient’s unique genetics, lifestyle, and health conditions, AI could one-day tailor medication regimens that minimize interaction risks and maximize therapeutic benefits.
Conclusion
Polypharmacy is both a necessary and risky reality of modern medicine. As patients live longer and develop more complex health conditions, the use of multiple medications is inevitable. However, the risks posed by drug interactions and ADRs cannot be ignored. Pharmacovigilance stands at the forefront of this issue, helping to detect, assess, and prevent the potentially harmful effects of polypharmacy.
For healthcare providers and patients alike, understanding these risks and utilizing the resources provided by pharmacovigilance systems can help manage the delicate balance of treating multiple conditions without compromising patient safety.